Early detection through breast self-exams and screening mammography is crucial for improving breast cancer survival rates. Be vigilant for warning signs like new lumps, nipple discharge, changes in breast shape or skin texture. Promptly reporting any abnormalities to a healthcare provider enables timely diagnostic testing and initiation of an appropriate treatment plan. Survival statistics underscore the lifesaving impact of early detection. Learn more about evidence-based screening guidelines, risk factors, and comprehensive breast cancer care through authoritative medical resources.
Key Takeaways
- Performing regular breast self-exams is crucial for early detection.
- Early signs include new lumps, nipple discharge, or skin changes.
- Promptly consult a doctor about any breast abnormalities detected.
- Early detection via screening improves survival and treatment outcomes.
- Mammograms and other imaging tests aid in breast cancer diagnosis.
Breast Lump Awareness
One of the most common symptoms of breast cancer is the presence of a new lump or mass in the breast or underarm area. It's crucial to be aware of any changes in the appearance or texture of your breasts, as early detection can significantly improve treatment outcomes.
The appearance of a lump can vary greatly. It may feel hard, tender, or movable under the skin. Some lumps are painless, while others may cause discomfort or pain. The size of the lump can range from small, pea-sized bumps to larger masses.
It's essential to conduct regular self-examinations and be familiar with the normal texture and shape of your breasts. If you notice any new lumps, changes in size or shape, skin dimpling, nipple retraction, or any other concerning symptoms, promptly consult your healthcare provider.
Nipple Discharge Symptoms
Another potential symptom of breast cancer is nipple discharge, which can occur spontaneously or with breast compression. It's important to be aware of any unusual fluid leaking from the nipple, as this could be an early sign of a problem.
- Spontaneous oozing or leaking of fluid from the nipple, without squeezing or pressure
- Discharge that is bloody, clear, or another abnormal color
- Nipple discharge that occurs from only one breast
Nipple discharge can have various causes, some benign and others more serious. However, if you experience any spontaneous nipple discharge, especially if it's bloody or coming from only one breast, it's crucial to have it evaluated by a healthcare professional promptly.
Early detection and proper diagnosis are key to effective treatment and better outcomes.
Breast Shape Changes
While nipple discharge warrants medical attention, breast shape changes can also signal potential breast cancer. One concerning sign is breast contour asymmetry, where one breast develops a noticeably different shape or size than the other. This may indicate a lump or mass within the breast tissue.
Nipple inversion changes, where the nipple begins to turn inward, can also be a warning sign. Normally, nipples point outward.
It's crucial to promptly report any breast or nipple changes to your healthcare provider. While these symptoms do not necessarily mean cancer, only further examination can determine the underlying cause.
Early detection greatly improves breast cancer treatment outcomes and survival rates. Performing regular self-exams and attending scheduled mammograms increase the chances of catching any abnormalities early when they are most treatable.
Don't delay reporting persistent breast changes – your health is the top priority.
Skin Texture Alterations
Skin texture changes around the breast area may indicate an underlying breast issue. Changes in the skin's appearance can sometimes be an early sign of breast cancer.
Here are some potential skin texture alterations to be aware of:
- Redness or scaliness of the skin
- Skin thickening or developing a 'pitted' or 'dimpled' appearance (pitting edema)
- The skin resembling an orange peel (dimpling appearance)
These changes may be caused by cancer cells blocking lymph vessels in the skin over the breast. This obstruction can lead to swelling and changes in the skin's texture and appearance.
It is crucial to be vigilant and report any unusual skin changes to your healthcare provider promptly. Early detection is key in the successful treatment of breast cancer. Routine breast self-exams and regular mammograms can help catch any concerning changes early when they are most treatable.
Do not hesitate to seek medical attention if you notice any skin texture alterations or other worrisome breast changes.
Performing Self-Exams
Regularly performing breast self-exams plays a crucial role in early detection of breast cancer. These self-checks allow you to become familiar with the normal look and feel of your breasts, making it easier to identify any changes that may occur. The recommended approach is to conduct a monthly inspection, typically a few days after your menstrual cycle, when breasts are least likely to be swollen or tender.
The process involves a thorough mirror check, visually inspecting both breasts for any changes in size, shape, or skin appearance while standing and raising your arms overhead.
Next, lie down and use the pads of your fingers to gently yet firmly palpate each breast in a circular motion, checking for any lumps, thickening, or unusual discharge from the nipples.
It's essential to examine the entire breast area, including the underarm region.
Mammogram Screening Guidelines
Mammogram screening guidelines help women understand when to start undergoing regular mammograms and how often they should be screened.
The American Cancer Society recommends annual mammograms starting at age 45 for women at average risk, with the option to begin annual screening as early as age 40.
Women aged 55 and older can transition to biennial (every two years) screening or continue with annual mammograms.
Age Recommendations
When should women begin receiving regular mammogram screenings for early breast cancer detection? This is an important question as mammography plays a crucial role in detecting breast cancer at its earliest, most treatable stages.
- Age 40: Most major health organizations recommend annual mammogram screenings starting at age 40 for women at average risk.
- Age 30: Women with a higher risk due to family history or other factors may need to start screening as early as age 30.
- Age 50-74: For women in this age range, mammograms are strongly recommended every 1-2 years, as the risk of breast cancer increases with age.
It's essential to follow age milestones and the risk timeline for mammogram screenings. These guidelines are based on extensive research and aim to balance the benefits of early detection with the potential risks of false positives and overdiagnosis.
Consult your healthcare provider to determine your personalized screening schedule based on your individual risk factors and preferences.
Screening Frequency
Adherence to recommended screening intervals optimizes the benefits of mammography for early breast cancer detection. The frequency of mammogram screenings depends on individual risk factors determined through comprehensive risk assessment. Women at average risk of breast cancer should commence annual screening mammograms at age 40 and continue annually until age 54.
After 55, screening intervals can transition to every two years or continue annually based on personal preferences and risk assessment. Women with elevated risk due to family history, genetic mutations, or other factors may require more frequent screenings, potentially starting before age 40. Consulting with a healthcare provider is crucial for determining appropriate screening intervals tailored to one's unique circumstances.
Early detection through adherence to recommended screening intervals significantly improves breast cancer outcomes. By following guidelines and maintaining open communication with medical professionals, women can proactively monitor their breast health and promptly address any potential concerns. Embracing an empowered approach to breast cancer screening is a proactive step towards safeguarding one's well-being.
Risk Factors Overview
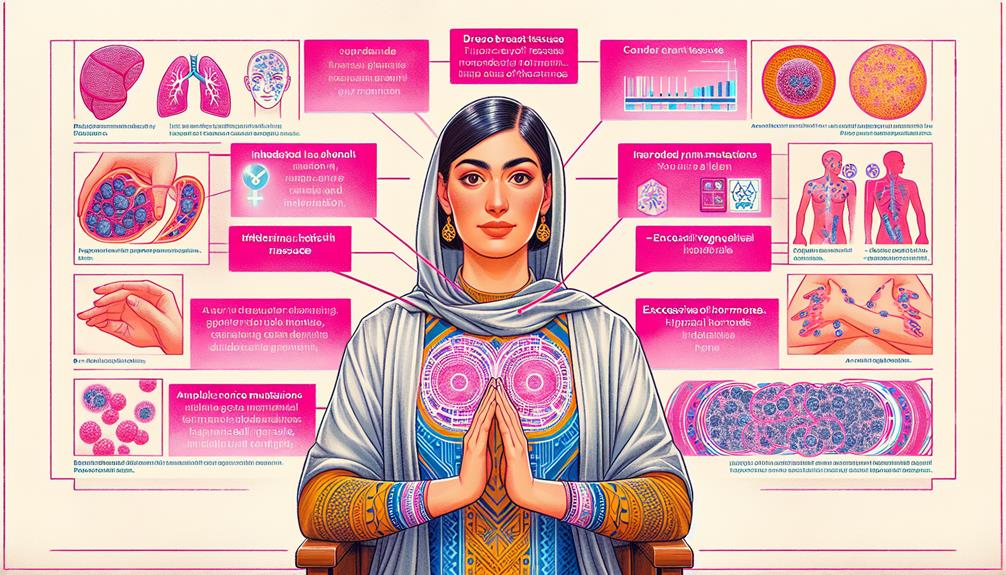
Age emerges as a principal risk factor for breast cancer, with the likelihood increasing substantially after age 40. However, it's crucial to be aware of other significant risk factors as well.
- Family history and genetic mutations play a vital role
- Certain lifestyle choices can influence the risk
- Hormonal and reproductive factors contribute to the equation
A family history of breast cancer or the presence of specific genetic mutations, such as in the BRCA1 and BRCA2 genes, can significantly increase an individual's risk. Additionally, lifestyle factors like obesity, lack of physical activity, and alcohol consumption have been linked to a higher incidence of breast cancer.
Hormonal and reproductive factors should not be overlooked. Early menstrual periods, late menopause, and not having children or breastfeeding can contribute to the risk.
It's essential to be proactive and undergo regular screenings, especially for those with known risk factors. Early detection and prompt treatment can greatly improve the chances of successful outcomes.
Diagnostic Testing Options
Early detection is crucial for effective breast cancer treatment. Mammography screening guidelines help identify those at risk, while biopsy testing, including fine needle aspiration and surgical biopsies, confirm the diagnosis.
Imaging tests like ultrasound, MRI, and nuclear medicine scans provide valuable information about tumor characteristics and spread.
Mammography Screening Guidelines
Mammography screening guidelines vary based on factors such as individual risk and organizational recommendations. Most major health organizations advise women at average risk to begin annual mammograms at age 40 or 45, with some recommending biennial screening after age 55. However, these guidelines remain controversial due to concerns about:
- Overdiagnosis and overtreatment of slow-growing cancers
- Potential harm from radiation exposure
- False-positive results leading to unnecessary procedures
For women at higher risk due to family history, genetic mutations, or other factors, earlier and more frequent screening may be advised. Ultimately, the decision should involve shared decision-making between patients and their healthcare providers, considering individual risk factors, preferences, and the potential benefits and harms of screening.
Biopsy Testing Types
If abnormalities are detected during screening or a patient presents with concerning breast findings, a biopsy may be recommended to obtain a sample of cells or tissue for further diagnostic evaluation.
There are several types of biopsy procedures used for breast tissue sampling, each involving different needle types and techniques.
A fine needle aspiration biopsy uses a very thin, hollow needle to extract a sample of cells from a lump or area of concern. This minimally invasive procedure can often be performed in the doctor's office.
A core needle biopsy utilizes a larger, hollow needle to remove a cylindrical sample of tissue for examination. Stereotactic, ultrasound, or MRI guidance may be employed to aid precise needle placement.
In some cases, a surgical biopsy may be necessary, involving the removal of part or all of the suspicious area during an outpatient procedure.
The tissue sample obtained through biopsy is then sent to a pathologist for comprehensive analysis to determine if cancer cells are present and identify specific characteristics that guide treatment recommendations.
Imaging Tests Available
In addition to physical examinations and biopsy procedures, various imaging tests are available to aid in the diagnosis and evaluation of breast abnormalities. These imaging techniques play a crucial role in the diagnostic process, helping healthcare professionals make informed decisions about treatment options.
Mammography: This low-dose X-ray examination remains the gold standard for breast cancer screening and detection.
Ultrasound: This non-invasive technique uses high-frequency sound waves to create detailed images of the breast tissue.
Magnetic Resonance Imaging (MRI): This advanced imaging modality provides highly detailed images of the breast, helping to differentiate between benign and malignant lesions.
Imaging tests are an essential part of the diagnostic journey, providing valuable information about the size, location, and characteristics of any breast abnormalities. By utilizing these advanced imaging techniques, healthcare professionals can develop personalized treatment plans tailored to each individual's needs, ensuring the best possible outcomes for those affected by breast cancer.
Treatment Plan Development

Developing a comprehensive treatment plan is crucial after a breast cancer diagnosis, tailored to the specific type, stage, and characteristics of the patient's cancer. The first step often involves a thorough discussion with a multidisciplinary team of healthcare professionals, including surgeons, medical oncologists, radiation oncologists, and other specialists.
The treatment plan may involve various modalities such as surgery, radiation therapy, chemotherapy, targeted therapy, hormone therapy, or a combination of these options. The surgery plan may include a lumpectomy (removal of the tumor and a small portion of surrounding tissue) or a mastectomy (removal of the entire breast).
Treatment options like chemotherapy, targeted therapy, and hormone therapy are frequently used to eliminate any remaining cancer cells and reduce the risk of recurrence. Throughout the process, patients are encouraged to actively participate in decision-making, considering factors like their overall health, personal preferences, and quality-of-life concerns.
Support services, such as counseling and nutritional guidance, are often integrated into the treatment plan to address the emotional and physical challenges that may arise.
Survival Rate Statistics
Survival rates for breast cancer vary significantly based on factors such as the stage of cancer at diagnosis, tumor characteristics, and the overall health of the patient.
According to the American Cancer Society, the 5-year relative survival rate for localized breast cancer is 99%, while the rate drops to 28% for metastatic breast cancer.
It is crucial to examine and understand these statistics to develop appropriate treatment strategies and provide accurate prognostic information to patients.
Survival Rate Data
Breast cancer's survival rate statistics provide valuable insights into the potential outcomes and prognosis for individuals diagnosed with this disease. According to the American Cancer Society, the relative 5-year survival rate for breast cancer is:
- 99% for localized breast cancer (confined to the breast)
- 86% for regional breast cancer (spread to nearby lymph nodes)
- 28% for distant breast cancer (metastasized to other organs)
These mortality rate data and prognosis statistics underscore the importance of early detection and timely treatment. The earlier breast cancer is detected and treated, the better the chances of survival and successful management.
It is crucial for women to be aware of breast cancer symptoms, perform regular self-examinations, and attend recommended screenings. By taking proactive measures and seeking medical attention promptly, individuals can increase their chances of catching the disease in its early stages, improving their overall prognosis and survival rate.
Statistics Breakdown
The survival rate statistics for breast cancer can be further broken down by factors such as stage at diagnosis, tumor grade, and molecular subtype. According to the American Cancer Society, the 5-year relative survival rate for localized breast cancer is 99%, while it drops to 28% for metastatic breast cancer.
Additionally, the incidence rates and mortality statistics vary based on the molecular subtype, with triple-negative breast cancer having poorer outcomes compared to hormone receptor-positive subtypes.
The age at diagnosis also plays a crucial role in breast cancer survival rates. Women diagnosed before age 40 tend to have more aggressive tumors and lower survival rates compared to older women. However, advancements in targeted therapies and early detection through regular screening have significantly improved survival rates across all age groups.
It is essential to understand these statistics to make informed decisions about treatment and follow-up care, as well as to prioritize efforts in reducing breast cancer incidence and mortality through awareness and prevention strategies.
Support Group Resources
Numerous support groups exist for individuals diagnosed with breast cancer, providing invaluable emotional support and resources. These groups offer a safe space to share experiences, cope with challenges, and connect with others going through similar journeys.
- Online forums and virtual communities allow for 24/7 access to support, regardless of location.
- In-person meetings foster a sense of community and face-to-face connections.
- Many organizations offer educational resources, counseling services, and community outreach programs.
Joining a support group can help alleviate feelings of isolation and provide a sense of belonging during a difficult time. Participants can share coping strategies, receive practical advice, and find strength in the shared experiences of others.
Both online forums and local community groups provide opportunities to build a supportive network, access valuable resources, and find empowerment through collective support.
Preventive Lifestyle Measures
In addition to seeking support, adopting specific lifestyle habits can play a role in breast cancer prevention. Maintaining a healthy weight, engaging in regular physical activity, and following a balanced diet rich in fruits, vegetables, and whole grains are recommended preventive measures. Exercise routine and dietary recommendations have been associated with a reduced risk of breast cancer. The following table summarizes key lifestyle factors and their potential impact on breast cancer risk:
| Factor | Recommendation |
|---|---|
| Body Weight | Maintain a healthy body mass index (BMI) |
| Physical Activity | Aim for at least 150 minutes of moderate exercise per week |
| Diet | Consume a plant-based diet rich in fiber, antioxidants, and healthy fats |
| Alcohol Consumption | Limit alcohol intake to no more than one drink per day |
While these lifestyle modifications cannot guarantee prevention, they can contribute to overall health and well-being, potentially reducing the risk of breast cancer and other chronic diseases. It's essential to consult with healthcare professionals for personalized guidance and to foster a sense of empowerment through informed decisions.
Frequently Asked Questions
Can Stress Cause Breast Cancer?
Stress alone does not cause breast cancer, but lifestyle factors and hormonal changes associated with chronic stress may increase risk. Taking steps to manage stress and maintain a healthy lifestyle is recommended for overall well-being and potentially reducing breast cancer risk.
Are There Genetic Screening Tests Available?
One in eight women will develop breast cancer. Yes, genetic screening tests involve genetic counseling and risk assessment to identify inherited mutations that increase cancer susceptibility, aiding prevention for high-risk individuals.
Is Breast Cancer Preventable Through Diet?
While there is no definitive dietary cure, following dietary recommendations emphasizing plant-based foods may slightly reduce breast cancer risk. However, adhering to screening guidelines remains crucial for early detection and risk reduction.
What Are the Emotional Impacts Experienced?
The emotional impacts often involve fear escalation and anxiety, necessitating coping mechanisms. Our compassionate community provides understanding and support during this challenging experience.
Are There Fertility Preservation Options?
Like a lighthouse guiding ships, fertility preservation options such as egg freezing and ovarian preservation offer hope for those facing life's storms. These empowering choices foster a sense of control and belonging during challenging times.
Conclusion
Catching breast cancer early could mean the difference between life and death. Routine self-exams and clinical screening are vital for detecting suspicious lumps, nipple discharge, or skin changes before tumors have a chance to spread.
Early detection coupled with prompt treatment significantly boosts survival rates. Though the road ahead may seem daunting, a wealth of support resources and preventive lifestyle adjustments can empower individuals on their journey towards renewed health and wellbeing.
Leave a Reply