Cancer treatment is undergoing a paradigm shift, driven by immunotherapies that leverage the immune system, targeted gene therapies tailored to molecular profiles, and personalized precision oncology approaches. Novel tumor-agnostic drugs target genetic mutations across cancer types, while nanoparticle delivery systems enhance specificity and minimize collateral damage. Liquid biopsies enable early detection and treatment monitoring, complemented by precision radiotherapy techniques. Artificial intelligence optimizes treatment planning, predicts outcomes, and streamlines clinical trials. Explore further to uncover the cutting-edge strategies reshaping the landscape of cancer care.
Key Takeaways
- Immunotherapies harness the body's immune system to combat cancer cells.
- Targeted gene therapies modify genes for tailored, potentially curative treatments.
- Personalized medicine matches patients with optimal therapies using molecular profiling.
- Novel delivery systems like nanoparticles enhance specificity and reduce side effects.
- AI integration optimizes radiotherapy planning, predicts outcomes, and streamlines clinical trials.
Immunotherapy Breakthroughs
A growing body of evidence supports the efficacy of immunotherapies, which leverage the body's own immune system to combat cancer. Immune checkpoint inhibition, a revolutionary form of immunotherapy, has emerged as a promising approach. By blocking specific proteins that act as 'brakes' on the immune response, these treatments unleash the body's natural defenses to recognize and attack malignant cells more effectively.
Monoclonal antibody treatment is another immunotherapy modality that has garnered significant attention. These engineered antibodies bind to specific targets on cancer cells, rendering them more susceptible to immune system elimination. By precisely harnessing the exquisite specificity of the immune system, monoclonal antibodies have demonstrated remarkable clinical outcomes, particularly in combination with other therapies.
As our understanding of the intricate interplay between the immune system and cancer deepens, immunotherapies offer a paradigm shift in cancer treatment. With their potential for durable responses, reduced toxicity, and improved quality of life, these innovative approaches hold the promise of transforming the landscape of oncology and fostering a sense of hope within the cancer community.
Targeted Gene Therapies
Complementing the advancements in immunotherapy, targeted gene therapies represent another frontier in the quest for more effective and personalized cancer treatments. These cutting-edge approaches leverage gene editing tools and viral vectors to precisely modify or introduce therapeutic genes into cancer cells or the patient's immune system.
The potential benefits of targeted gene therapies are multifaceted:
- Tailored to an individual's genetic makeup, enhancing treatment efficacy
- Minimizing collateral damage to healthy cells, reducing side effects
- Targeting specific molecular pathways driving tumor growth and metastasis
- Enhancing the patient's immune response against cancer cells
- Offering a durable, potentially curative solution for certain malignancies
While still in the early stages of clinical development, targeted gene therapies hold immense promise for our community of patients and researchers alike.
As we continue to unravel the complex genomic landscape of cancer, these innovative therapies may pave the way for a future where cancer is treated with unprecedented precision and personalization.
Personalized Medicine Advancements

Personalized medicine – the tailoring of treatment strategies based on an individual's unique genetic, molecular, and clinical profile – represents a paradigm shift in cancer care, fueled by remarkable advancements in genomics, proteomics, and bioinformatics. Biomarker discovery and genomic profiling have enabled the identification of specific molecular alterations that drive tumor growth and metastasis.
This knowledge has paved the way for the development of targeted therapies that selectively inhibit these aberrant pathways, offering a more precise and effective approach compared to traditional cytotoxic chemotherapies. By harnessing the power of precision oncology, clinicians can match patients with the most appropriate treatment regimen, minimizing unnecessary toxicities and maximizing therapeutic efficacy.
Furthermore, ongoing research efforts are focused on integrating multi-omics data, leveraging artificial intelligence algorithms, and developing novel diagnostic tools to further refine treatment selection and monitoring. As our understanding of cancer biology deepens, personalized medicine holds the promise of transforming patient outcomes and ushering in a new era of cancer care.
Tumor-Agnostic Drug Development
A paradigm shift in oncology has witnessed the emergence of tumor-agnostic drug development, where therapies target specific genetic mutations across various cancer types, rather than being confined to a particular tumor site.
This targeted approach leverages genetic marker analysis to identify patients most likely to benefit from a given treatment.
Clinical trials have demonstrated promising outcomes with tumor-agnostic therapies, paving the way for a more personalized and precise approach to cancer management.
Targeted Therapy Approach
Tumor-agnostic therapy, an emerging paradigm in cancer treatment, leverages molecular insights to selectively target driver mutations across diverse cancer types. This targeted therapy approach represents a shift from traditional organ-specific cancer treatment, focusing instead on the molecular underpinnings of malignancy.
The advantages of targeted therapy are multifaceted:
- Precision targeting of cancer-driving mutations
- Improved therapeutic index and reduced off-target toxicities
- Potential to overcome drug resistance mechanisms
- Applicability across multiple tumor types
- Personalized medicine tailored to individual patient profiles
The advent of next-generation sequencing and comprehensive molecular profiling has facilitated the identification of actionable targets, paving the way for receptor targeting and pathway inhibition strategies.
Genetic Marker Analysis
The identification of clinically actionable genetic alterations across diverse tumor types underpins the paradigm shift towards tumor-agnostic therapies. Comprehensive genomic profiling with extensive biomarker panels enables the detection of recurrent mutational signatures and molecular subtypes that transcend traditional histological classifications. This approach has catalyzed the development of precision oncology drugs targeting shared genetic drivers, irrespective of the tissue of origin.
Emerging strategies leverage machine learning algorithms to integrate multi-omics data, uncovering novel vulnerabilities and synergistic combinations tailored to an individual's tumor molecular landscape.
Basket trials evaluating the efficacy of targeted agents across tumor types harboring specific genetic aberrations have demonstrated promising outcomes, paving the way for regulatory approvals and reimbursement models aligned with this tumor-agnostic paradigm.
Ultimately, genetic marker analysis empowers clinicians to precisely match patients with the most appropriate targeted therapies, optimizing therapeutic responses while minimizing unnecessary toxicities, thereby advancing personalized cancer care.
Clinical Trial Advancements
Several pioneering clinical trials have spearheaded the evaluation of tumor-agnostic therapies targeting shared molecular drivers across diverse cancer types. These innovative approaches hold immense promise for transforming cancer treatment paradigms, transcending traditional organ-based silos.
Significant advancements in clinical trial design and implementation include:
- Basket trials: Enrolling patients with various tumor types harboring a shared molecular alteration, enabling simultaneous assessment of targeted therapies across multiple malignancies.
- Umbrella trials: Evaluating multiple targeted therapies within a single disease type, facilitating efficient exploration of multiple treatment options for patient subgroups.
- Master protocols: Adaptive trial platforms allowing for seamless addition or removal of investigational arms based on accruing data, optimizing patient accrual and expediting progress.
- Biomarker-driven stratification: Leveraging genetic marker analysis to enrich patient populations most likely to benefit, enhancing therapeutic signal detection.
- Rigorous toxicity management strategies: Proactive approaches to mitigate and address treatment-related adverse events, ensuring patient safety.
Despite patient accrual challenges, these innovative trial designs hold the key to accelerating the development of precision oncology therapies, unlocking new horizons in cancer care.
Nanoparticle Delivery Systems
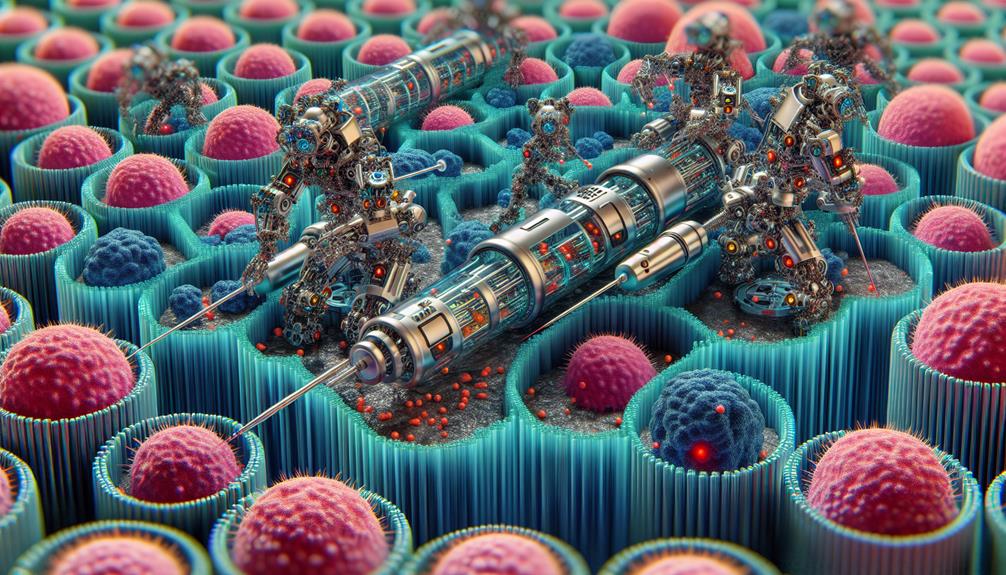
Emerging as a promising avenue in cancer treatment, nanoparticle delivery systems leverage biocompatible materials engineered at the nanoscale to precisely target and deliver therapeutic agents to malignant cells. These innovative systems offer enhanced specificity and efficacy, minimizing collateral damage to healthy tissues.
One approach involves nanobot transport, where minuscule robotic vehicles navigate the body, guided by advanced imaging techniques, to reach tumor sites and administer potent payloads. Alternatively, nanocarrier encapsulation employs nanoscale capsules tailored to encapsulate chemotherapeutic drugs or genetic material, shielding them from degradation and facilitating controlled release at the desired location.
Through meticulous design and rigorous clinical evaluation, nanoparticle delivery systems hold the potential to revolutionize cancer therapy, offering personalized, targeted regimens that align with the shared pursuit of improved patient outcomes and higher quality of life for those afflicted by this formidable disease.
Cancer Stem Cell Targeting
Cancer stem cells possess remarkable plasticity, enabling them to evade conventional therapies and drive tumor progression.
Targeting cancer stem cells could potentially enhance treatment efficacy by eliminating the root source of malignancy.
Novel strategies exploiting the unique properties of cancer stem cells hold promise for developing targeted therapies that may improve patient outcomes.
Stem Cell Plasticity
One promising avenue for novel cancer therapies lies in targeting stem cell plasticity, exploiting the unique properties of cancer stem cells. These cells possess remarkable plasticity, allowing them to transition between different cell states and contribute to tumor heterogeneity and treatment resistance.
By understanding the mechanisms underlying stem cell plasticity, researchers aim to develop targeted therapies that can effectively target and eliminate these resilient cells.
Potential strategies in this area include:
- Targeting cell reprogramming pathways that regulate stem cell plasticity
- Exploiting pluripotency models to identify vulnerabilities in cancer stem cells
- Developing therapies that inhibit the transition between stem-like and non-stem-like states
- Exploring epigenetic regulators that influence stem cell plasticity
- Combining stem cell-targeting agents with conventional therapies for enhanced efficacy
Harnessing stem cell plasticity holds great promise for improving cancer treatment outcomes. By targeting the dynamic nature of cancer stem cells, researchers strive to develop more effective and personalized therapeutic approaches, ultimately leading to better patient outcomes and increased chances of long-term remission.
Targeted Therapies Potential
Building upon the potential of targeting stem cell plasticity, a promising approach involves developing targeted therapies that specifically modulate or eliminate cancer stem cells. Rational combinations of targeted agents, such as kinase inhibitors, hold immense potential in disrupting the intricate signaling pathways that govern cancer stem cell survival, self-renewal, and therapeutic resistance. By precisely targeting these critical drivers of tumor progression, targeted therapies offer a more selective and personalized approach to cancer treatment.
The advent of precision medicine and the growing understanding of cancer stem cell biology have paved the way for the development of targeted therapies. These innovative strategies aim to exploit the unique molecular vulnerabilities of cancer stem cells, minimizing collateral damage to healthy tissues. By rationally combining targeted agents with complementary mechanisms of action, researchers strive to overcome redundancy and augment therapeutic efficacy, ultimately enhancing clinical outcomes for patients.
Epigenetic Therapy Innovations
Recent advancements in epigenetic research have paved the way for innovative therapeutic approaches that address the complex interplay between genetic and environmental factors contributing to cancer development and progression. Epigenetic therapy holds immense promise in our collective fight against cancer, offering a personalized and targeted approach to treatment.
The field of epigenetic therapy encompasses:
- Epigenetic drug development: Designing drugs that modulate the epigenetic landscape, such as histone deacetylase inhibitors and DNA methyltransferase inhibitors, to restore normal gene expression patterns.
- Epigenetic biomarker identification: Identifying epigenetic signatures that can serve as diagnostic and prognostic markers, guiding treatment decisions and monitoring treatment responses.
- Combination therapies: Combining epigenetic therapies with existing cancer treatments to enhance efficacy and overcome resistance mechanisms.
- Precision medicine: Tailoring epigenetic therapies based on an individual's unique epigenetic profile, enabling personalized treatment strategies.
- Preventative measures: Exploring the potential of epigenetic interventions in cancer prevention by targeting epigenetic mechanisms implicated in early carcinogenesis.
With ongoing research and clinical trials, epigenetic therapy holds the potential to revolutionize cancer treatment, offering hope and belonging to those affected by this devastating disease.
Tumor Microenvironment Modulation
Tumor microenvironment modulation encompasses innovative strategies targeting immune cells and metabolic pathways within the tumor's complex ecosystem.
Immune cell targeting aims to harness the body's defense mechanisms by modulating checkpoint inhibitors or leveraging adoptive cell therapies.
Simultaneously, metabolic pathway manipulation seeks to disrupt the intricate metabolic circuits fueling tumor growth and survival, potentially sensitizing cancer cells to other therapies.
Immune Cell Targeting
Exploiting the tumor microenvironment through modulation of immune cell activity represents a promising therapeutic strategy in cancer treatment. Immune cell targeting aims to harness the body's natural defense mechanisms to combat malignancies effectively.
This approach encompasses various techniques, including:
- Immune checkpoint inhibition
- Adoptive cell transfer therapy
- Oncolytic virus therapy
- Immune cell engineering
- Immune profiling and personalized immunotherapies
Metabolic Pathway Manipulation
A promising strategy in cancer therapy involves manipulating the metabolic pathways within the tumor microenvironment to disrupt the intricate network supporting tumor growth and progression. Cancer cells undergo metabolic reprogramming, altering their energy production and biosynthetic pathways to meet the increased demands of rapid proliferation.
By targeting these metabolic dependencies, researchers aim to selectively starve cancer cells of essential nutrients, ultimately inducing cell death or impeding their ability to thrive.
One approach is to exploit the tumor's heightened glycolytic activity, known as the Warburg effect, by inhibiting glycolysis or disrupting the supply of glucose and other nutrients. Another strategy involves targeting metabolic enzymes or transporters crucial for cancer cell survival, inducing nutrient deprivation and metabolic stress.
Additionally, modulating the tumor microenvironment's acidity, hypoxia, or immune cell infiltration can indirectly influence cancer cell metabolism and disrupt the delicate balance required for tumor sustenance. By uncovering and targeting these metabolic vulnerabilities, researchers strive to develop more effective and selective cancer treatments tailored to each patient's unique tumor biology.
Liquid Biopsy Diagnostics

Liquid biopsy diagnostics, representing a minimally invasive approach, facilitate the analysis of circulating tumor DNA and tumor cells shed into bodily fluids, offering a promising avenue for early cancer detection, monitoring treatment response, and tracking tumor evolution.
These cutting-edge techniques have the potential to revolutionize cancer management by providing valuable insights into the molecular landscape of the disease.
Key advantages of liquid biopsy diagnostics include:
- Early detection of cancers through the identification of specific blood biomarkers
- Personalized cancer screening and monitoring, reducing the need for invasive tissue biopsies
- Real-time tracking of tumor evolution and treatment response
- Identification of resistance mechanisms and potential therapeutic targets
- Improved patient outcomes through timely interventions and tailored treatment strategies
Radiotherapy Precision Enhancements
Complementing the advancements in liquid biopsy diagnostics, radiotherapy precision enhancements represent another frontier in optimizing cancer treatment modalities. Radiation oncologists are leveraging technological innovations to precisely target malignant tissues while minimizing collateral damage to surrounding healthy cells. Radiation dose optimization algorithms and advanced collimator engineering enable conformal radiation delivery, tailoring the beam intensity and shaping it to the tumor's contours.
| Technique | Benefit | Applications |
|---|---|---|
| Intensity-Modulated Radiotherapy (IMRT) | Sculpts radiation dose | Head and neck, prostate, and breast cancers |
| Stereotactic Body Radiotherapy (SBRT) | Precisely targets tumors with high-dose radiation | Early-stage lung cancer, liver metastases |
| Proton Beam Therapy | Minimal exit dose beyond tumor | Pediatric cancers, tumors near critical structures |
These advancements have revolutionized radiation oncology, enabling clinicians to maximize tumor control while preserving quality of life for patients. As we continue to refine radiotherapy techniques, we move closer to achieving personalized, targeted cancer treatment plans tailored to each individual's unique needs.
Artificial Intelligence Integration
Catalyzing the integration of artificial intelligence (AI) into cancer treatment protocols, machine learning algorithms are being leveraged to optimize radiotherapy planning and delivery. AI data mining and machine learning algorithms enable the analysis of vast patient datasets, facilitating personalized treatment strategies tailored to individual tumor characteristics and response patterns. This precision oncology approach holds immense potential for enhancing therapeutic efficacy while minimizing collateral damage to healthy tissues.
The transformative potential of AI integration spans:
- Automated tumor segmentation and contouring
- Adaptive treatment planning based on real-time patient data
- Predictive modeling of treatment outcomes and toxicity risks
- Identification of optimal radiotherapy dose distributions
- Integration of multimodal data for holistic patient profiling
Clinical Trial Redesigns
Redesigning clinical trials with AI-enabled methodologies stands as a pivotal strategy to expedite the validation and translation of novel cancer therapies. Leveraging AI's capabilities in data analysis and pattern recognition, researchers can optimize trial recruitment by identifying eligible participants more efficiently and tailoring enrollment criteria. This targeted approach enhances trial diversity, ensuring a representative patient population and improving the generalizability of findings.
Furthermore, AI-driven protocol redesign can streamline trial processes, reducing operational complexities and minimizing patient burden. By automating data collection, monitoring, and analysis, AI solutions can identify potential safety concerns or efficacy signals earlier, enabling timely adaptations to trial protocols. This agile approach maximizes the likelihood of successful outcomes and accelerates the delivery of promising treatments to patients in need.
Ultimately, the integration of AI in clinical trial redesigns fosters a patient-centric paradigm, where trials are conducted with increased efficiency, rigor, and inclusivity. By harnessing the power of AI, the oncology community can drive transformative advancements in cancer care, offering hope and improved outcomes for patients worldwide.
Frequently Asked Questions
What Are the Potential Side Effects?
Potential side effects of cancer treatment involving the immune response or genetic predisposition may include fatigue, nausea, and increased susceptibility to infections. A personalized approach based on scientific evidence and clinical trials is crucial for optimal outcomes.
How Accessible Are These Treatments Financially?
The financial accessibility of treatments remains a daunting challenge – the cost burden can be substantial, often straining even robust insurance coverage. However, navigating this labyrinth together fosters a sense of solidarity in our shared pursuit of healing.
What Are the Success Rates so Far?
Preliminary data from ongoing clinical trials suggest promising success rates for innovative cancer treatments, offering renewed hope for patients seeking effective therapeutic options within a supportive medical community.
Are There Any Alternative/Complementary Therapies Available?
Consider a cancer patient exploring herbal remedies and lifestyle changes alongside conventional treatment. Yes, many patients seek alternative/complementary therapies, though efficacy evidence varies for such integrative approaches.
How Can Patients Get Involved in Trials?
Patients can explore online resources and connect with patient advocacy groups to learn about eligibility criteria and find appropriate clinical trials in their area. This approach fosters a sense of community while pursuing evidence-based treatment options.
Conclusion
The continuous evolution of cancer treatment modalities holds immense promise for improving patient outcomes and survival rates.
While challenges persist, ongoing research into novel therapies, precision medicine, and integrative technologies underscores the relentless pursuit to conquer this formidable disease.
The future of oncology hinges on seamlessly translating scientific breakthroughs into clinical practice, ultimately offering hope and better quality of life for those affected.
Leave a Reply